Let’s talk about something that often feels confusing and painful when you are trying to get pregnant. You do everything right. Tests look fine. Embryos are healthy. Still, pregnancy does not happen. Many people reach this point and feel stuck, not knowing what else could be wrong.
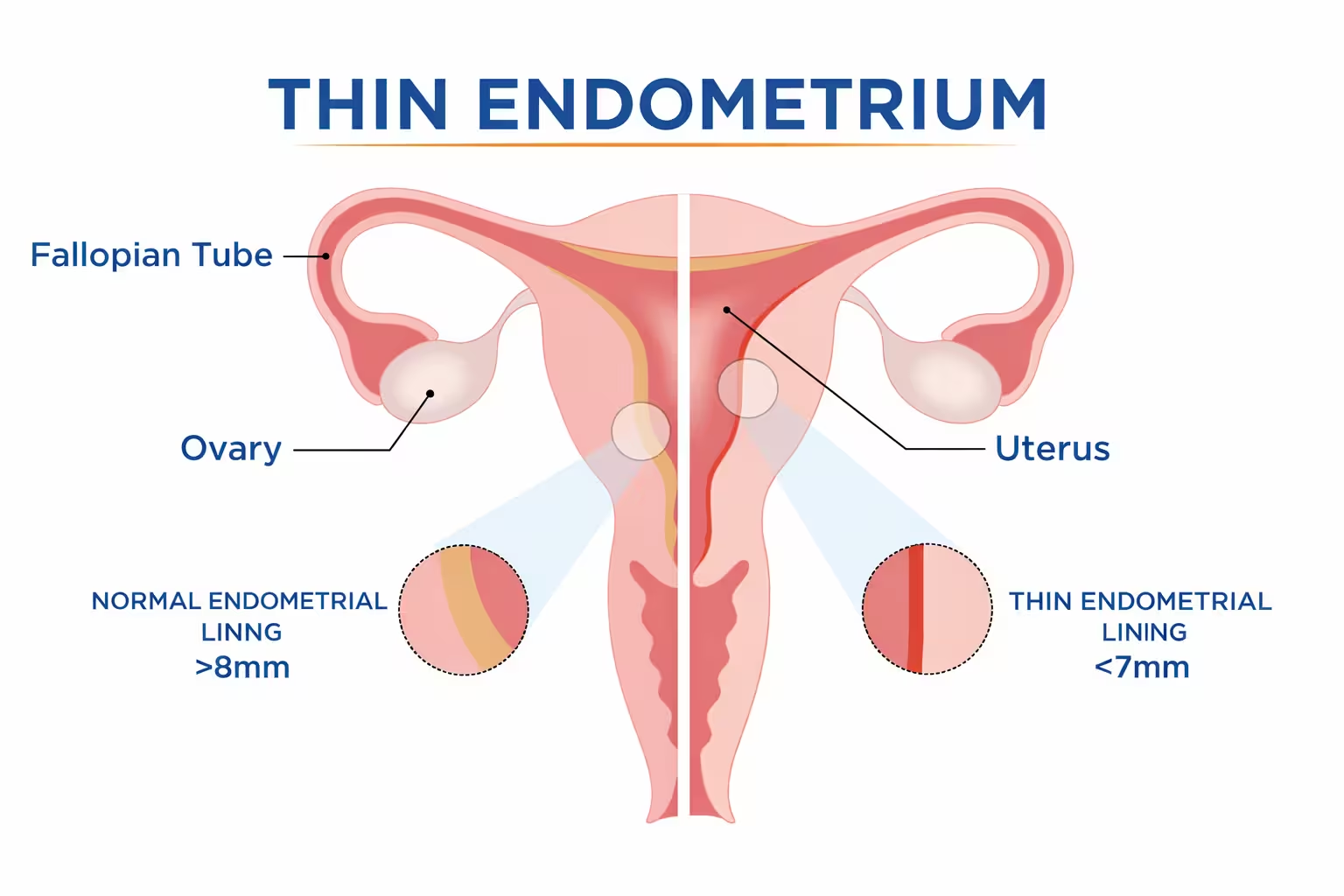
This is where thin endometrium and pregnancy come into the picture. The uterus plays a bigger role than most people realise. Even a good embryo needs the right place to settle. If the lining inside the uterus is too thin, the embryo may not attach or may stop developing very early. I think this part is not explained clearly enough during treatment.
A thin uterine lining does not provide enough support for implantation. Blood flow can be low. Hormone signals may not work in sync. To put it simply, the embryo arrives, but the body is not fully ready to receive it. You know, it can feel unfair, especially when everything else seems perfect. According to Mayo Clinic, the endometrium is essential for implantation, and problems with its health or development can affect the chances of pregnancy.
Many people hear the term implantation failure with good embryos and immediately feel hopeless. But this does not always mean something is permanently wrong. It often means the lining needs attention, time, and the right approach.
Understanding Thin Endometrium and Pregnancy
Before getting into treatments or outcomes, it helps to understand what thin endometrium and pregnancy really mean together. Many people focus only on eggs and embryos, but the uterus plays an equal role. If the lining inside the uterus does not grow well, pregnancy can struggle from the very beginning. This part often goes unnoticed because reports may say things look acceptable, even when they are not ideal.
A thin uterine lining can quietly lower the chance of implantation. At the same time, endometrial thickness for implantation decides whether the embryo feels supported enough to attach and continue growing. Once you understand this link, many confusing results from natural cycles or IVF start to feel less mysterious.
What Is a Thin Uterine Lining in Thin Endometrium and Pregnancy
A thin uterine lining means the inner layer of the uterus does not thicken enough during the cycle. This lining is where the embryo settles after fertilisation. In cases linked to thin endometrium and pregnancy difficulties, the lining often stays underdeveloped even when medicines are used.
When the lining is thin, it may appear smooth on scans but lack depth and strength. This makes it harder for the embryo to stay attached.
Some key things to keep in mind are:
- The lining grows mainly under the effect of estrogen
- Healthy blood flow helps the lining stay soft and supportive
- A thin uterine lining can look normal but still not work well
- The same pattern may repeat across cycles
Many people blame themselves or the embryo, but often the body is just not responding the way it should. Thin endometrium and pregnancy issues are usually about readiness, not personal failure.
Endometrial Thickness for Implantation and Early Pregnancy
Endometrial thickness for implantation is one of the most talked about factors in fertility care. Doctors often measure it before ovulation or embryo transfer. Still, the numbers can feel confusing if no one explains what they truly mean.
In simple words, the lining needs enough thickness to support the embryo in its earliest days. If it stays thin, implantation may not hold well.
What usually matters includes:
- The lining should grow gradually during the cycle
- Endometrial thickness for implantation depends on hormones and blood flow
- Pregnancy can happen with lower thickness, but chances reduce
- Early pregnancy needs both thickness and good lining quality
You might wonder why some people conceive with thin lining while others do not. Often, the answer lies in overall uterine health, not just one scan value.
Why Thin Endometrium and Pregnancy Outcomes Depend on the Lining
Thin endometrium and pregnancy outcomes depend heavily on how welcoming the lining is. Even when embryos are healthy, implantation may fail if the lining cannot hold or nourish them. This is why implantation failure with good embryos is often linked to uterine factors rather than embryo quality.
The lining works like a foundation. If it is weak, stability becomes difficult.
Important factors include:
- Steady blood supply reaching the lining
- Hormones arriving at the right time
- The lining remaining stable after implantation
- Low inflammation inside the uterus
A thin uterine lining does not mean pregnancy is impossible. It means the plan may need to change. Once this connection becomes clear, decisions feel calmer and more informed.
Why Implantation Fails Even With Good Embryos in Thin Endometrium and Pregnancy
It can feel deeply confusing when doctors say the embryos look good, yet pregnancy still does not happen. Many people reach this stage and start questioning everything. In reality, thin endometrium problems often explain this gap. Implantation is not only about the embryo arriving. It is also about whether the uterus is truly ready to receive it.
When the lining is thin, the embryo may try to attach but fail to settle properly. This can happen silently, without pain or clear signs. Implantation failure with good embryos is often linked to the uterine environment rather than the embryo itself. Once you understand this, the situation feels less mysterious and less personal.
Implantation Failure With Good Embryos and Thin Endometrium
Implantation failure with good embryos happens when the embryo cannot attach firmly to the uterine wall. In thin endometrium and pregnancy struggles, the lining does not provide enough depth or nourishment for the embryo to stay.
Even strong embryos need support in the first few days. Without it, they may stop developing very early.
Some important points to understand are:
- The embryo needs a soft, well prepared surface to attach
- Thin endometrium can reduce the grip needed for implantation
- Implantation failure with good embryos is often repeated across cycles
- Embryo quality alone cannot overcome a weak lining
This does not mean something is permanently wrong. It means the uterus needs more attention before expecting success.
Blood Flow Problems in Thin Uterine Lining Affecting Pregnancy
Blood flow plays a big role in how the uterus prepares for pregnancy. In a thin uterine lining, blood supply may be low or uneven. This affects how nutrients and oxygen reach the lining.
When blood flow is poor, endometrial thickness for implantation may not improve even with medication. The lining stays thin and less responsive.
Things that often matter here include:
- Healthy blood vessels supporting the uterine wall
- Oxygen reaching the lining at the right time
- Thin uterine lining linked to weak circulation
- Stress and lifestyle affecting blood flow
Improving blood flow is often a key step when thin endometrium and pregnancy do not move forward as expected.
Hormonal Timing Issues in Thin Endometrium and Pregnancy
Hormones guide the entire implantation process. In thin endometrium cases, hormone signals may arrive too early, too late, or not strongly enough. This creates a timing mismatch.
Endometrial thickness for implantation depends on estrogen and progesterone working in balance. If this balance is off, the lining may look fine on one day and become unstable the next.
Key points to keep in mind are:
- Estrogen supports lining growth
- Progesterone prepares the lining for implantation
- Endometrial thickness for implantation depends on correct timing
- Hormonal shifts can cause early implantation failure
When hormones and lining are not in sync, even the best embryo can miss its chance. Understanding this helps you focus on fixing the root issue instead of blaming outcomes.
Common Causes of Thin Uterine Lining and Pregnancy Failure
When pregnancy does not happen again and again, many people assume it is bad luck or poor embryo quality. But very often, the real reasons sit quietly in the background. Thin endometrium and pregnancy problems usually develop over time and are linked to things the body has been struggling with for a while.
A thin uterine lining does not appear suddenly. It is usually the result of hormonal issues, physical changes inside the uterus, or daily habits that slowly affect uterine health. Implantation failure with good embryos can happen when these causes are not identified early. Understanding them helps you stop guessing and start addressing the real problem.
Hormonal Imbalance in Thin Endometrium and Pregnancy
Hormones control how the uterine lining grows and prepares for pregnancy. In thin endometrium and pregnancy challenges, hormone levels may exist, but the body does not respond properly to them. This is more common than people realise.
Estrogen helps the lining grow, while progesterone helps it stay stable. If this balance is disturbed, the lining may remain thin or unstable.
Common hormonal issues include:
- Weak response to estrogen even when levels seem normal
- Progesterone rising too early or too late
- Endometrial thickness for implantation not improving across cycles
- Irregular cycles affecting lining growth
Thin endometrium and pregnancy problems linked to hormones are often treatable once timing and dosage are adjusted correctly.
Uterine Damage Leading to Thin Uterine Lining
Sometimes the uterus has been through procedures or infections that affect the lining. This damage may not cause pain, but it can stop the lining from growing properly. A thin uterine lining caused by damage often does not respond well to routine medicines.
This is one reason implantation failure with good embryos keeps repeating without clear answers.
Possible causes include:
- Past uterine surgeries or repeated procedures
- Scar tissue forming inside the uterus
- Infections that healed but left inflammation behind
- Thin uterine lining that stays the same every cycle
In these cases, the focus shifts from embryos to repairing or supporting the uterine environment.
Lifestyle and Stress Effects on Thin Endometrium and Pregnancy
Daily habits play a bigger role than most people expect. Thin endometrium and pregnancy outcomes can be affected by stress, poor sleep, nutrition gaps, and physical exhaustion. These factors slowly reduce blood flow and hormone balance.
Endometrial thickness for implantation depends not only on medicine but also on how the body feels overall.
Things that often matter are:
- Long term stress affecting hormone signals
- Poor sleep disturbing cycle rhythm
- Low iron or nutrition affecting blood supply
- Lack of rest reducing uterine recovery
Thin endometrium and pregnancy issues linked to lifestyle do not improve overnight. But small, steady changes often make the lining more responsive over time.
Endometrial Thickness for Implantation and Pregnancy Success
When people talk about fertility reports, one number comes up again and again. That number is endometrial thickness for implantation. It can feel stressful when scans focus so much on this single detail. Still, this measurement gives important clues about how ready the uterus is for pregnancy.
Thin endometrium and pregnancy outcomes are closely linked to how well the lining grows during a cycle. If the lining stays thin, implantation becomes harder even if everything else looks fine. Endometrial thickness for implantation helps doctors decide whether the body is ready to move forward or needs more time and support.
Minimum Endometrial Thickness for Implantation
Many people ask what the minimum endometrial thickness for implantation should be. The answer is not always the same for everyone, but there are general patterns doctors look for. Endometrial thickness for implantation reflects how much support the lining can give to an embryo.
When the lining stays below the expected range, the chances of stable implantation reduce. This does not mean pregnancy cannot happen, but it does mean the risk of early loss is higher.
Important points to understand include:
- Endometrial thickness for implantation usually increases steadily before ovulation or transfer
- A thicker lining often has better blood flow and hormone response
- Endometrial thickness for implantation is about quality, not just numbers
- Some bodies need more time to build lining safely
Focusing only on the number can be confusing. The goal is a lining that feels ready, stable, and well supported.
Can Pregnancy Happen With Thin Endometrium?
This is one of the most common and emotional questions people ask. Can pregnancy happen when the lining is thin? The honest answer is yes, it can happen, but it is not always easy. Thin endometrium and pregnancy can exist together, but the chances depend on many factors.
Some people conceive with a thin uterine lining because blood flow is good or hormones stay balanced. Others face implantation failure with good embryos because the lining cannot support growth for long.
Things that influence outcomes include:
- Overall uterine health beyond thickness
- Blood supply reaching the lining
- Hormonal balance during implantation days
- Thin uterine lining behaving differently in each cycle
Thin endometrium and pregnancy do not follow fixed rules. Understanding your body’s pattern helps you choose safer and more realistic next steps.
Treatment Options for Thin Endometrium and Pregnancy
When you hear that the lining is thin, it can feel discouraging. But the good news is that thin endometrium and pregnancy challenges often respond to the right kind of support. Treatment is not about forcing the body. It is about helping it respond in a healthier way. Different people need different approaches, and that is completely normal.
A thin uterine lining may improve with medical help, better blood flow, or simple lifestyle changes. Endometrial thickness for implantation can increase when the body feels safe, supported, and balanced. The key is patience and choosing steps that suit your body rather than rushing into the next cycle.
Medical Treatments for Thin Endometrium and Pregnancy
Medical treatment often focuses on helping the lining grow and stay stable. In thin endometrium and pregnancy care, doctors usually start by supporting hormones and lining response. Medicines are adjusted based on how your body reacts, not just on standard doses.
Endometrial thickness for implantation may improve slowly, and that is okay. What matters is steady progress rather than quick fixes.
Common medical approaches include:
- Estrogen support to encourage lining growth
- Adjusting hormone timing to match your cycle
- Monitoring endometrial thickness for implantation closely
- Giving the body extra time when response is slow
Thin endometrium and pregnancy treatment works best when medicines are personalised instead of repeated blindly.
Improving Blood Flow in Thin Uterine Lining
Blood flow plays a big role in lining health. A thin uterine lining often struggles because blood supply is weak or uneven. Without good blood flow, even strong medicines may not work well. This is why many treatment plans focus on circulation.
Better blood flow helps oxygen and nutrients reach the uterus, making the lining more responsive. It can also reduce implantation failure with good embryos.
Ways blood flow is supported include:
- Gentle movement that improves pelvic circulation
- Reducing long periods of stress and tension
- Treatments that relax uterine blood vessels
- Supporting overall heart and vascular health
Improving blood flow does not always give instant results, but it often makes the lining more receptive over time.
Lifestyle Support for Endometrial Thickness for Implantation
Lifestyle support is often underestimated, but it matters deeply. Endometrial thickness for implantation depends not only on medicines but also on how the body feels every day. Sleep, food, stress, and rest all send signals to the uterus.
Small changes can slowly improve how the lining responds during each cycle.
Helpful lifestyle factors include:
- Regular sleep to support hormone rhythm
- Balanced meals that support blood health
- Gentle activity to keep circulation steady
- Reducing mental pressure during treatment
Endometrial thickness for implantation improves best when medical care and daily habits work together. Thin endometrium and pregnancy outcomes often change when the body feels supported rather than pushed.
Conclusion
Thin endometrium and pregnancy issues can feel confusing and exhausting, especially when embryos look healthy. But this problem is more common than people realise, and it does not mean your journey is over. A thin uterine lining is often the body’s way of asking for better timing, support, or care. Once you understand what affects the lining, decisions become clearer and less stressful. With the right approach, patience, and support, many people do find a better path forward. I think the most important thing is to stop blaming yourself and start listening to what your body needs.
FAQs
Can pregnancy happen with thin endometrium?
Yes, it can happen, but chances depend on blood flow, hormones, and overall uterine health.
What is a safe endometrial thickness for implantation?
There is no single perfect number, but a thicker, well-supported lining improves stability.
Why do good embryos fail to implant?
Often because the uterine lining is not ready, not because of embryo quality.
Can thin uterine lining be improved?
In many cases, yes, with the right medical care, blood flow support, and lifestyle changes.